Who Touched My Medication? Why Record-Keeping in Disability Support Isn’t Optional
There are moments in this line of work that stop you cold. Moments when you think, Surely this can’t be happening—but it is.
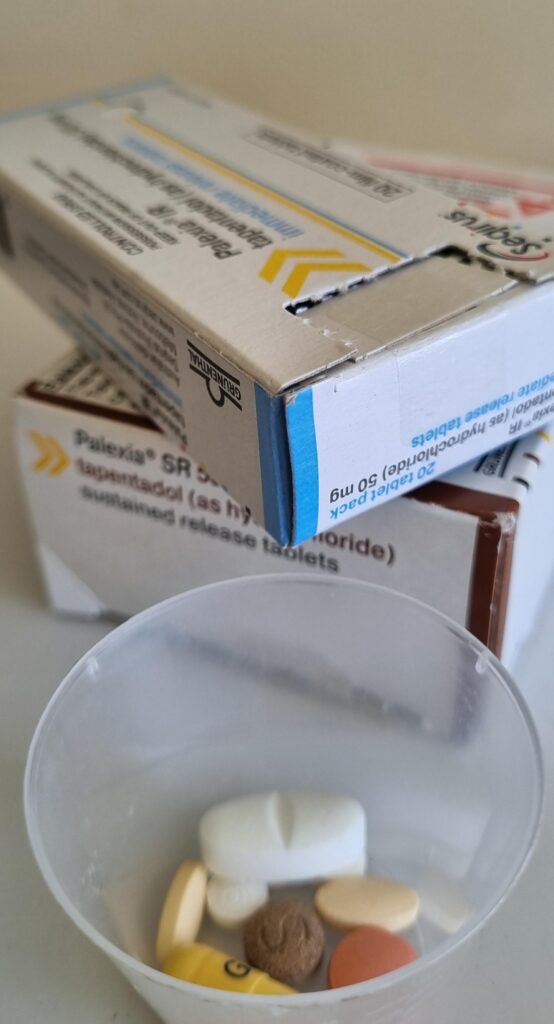
Recently, I sat down with a participant who relies on daily administration of controlled medication. They are supported by a team of disability support workers, all assigned to help with high-intensity, complex needs. On paper, everything seemed fine.
But when I asked how the medication was being tracked, the answer made my heart sink.
“We don’t document it. We were told not to sign anything medication-related if we’re not trained.”
Wait—what?
So instead of training the staff, the solution was to ignore record-keeping altogether?
No signatures. No records. No accountability.
When There’s No Record, There’s No Responsibility
Let’s be clear: this wasn’t just a casual oversight. This was a serious breakdown in basic care standards.
Not only was the medication not being documented, but the shift notes weren’t being completed either. For a high-intensity participant, this isn’t just concerning, it’s dangerous.
This isn’t about ticking boxes. It’s about building transparency, safety, and trust into every aspect of care.
If something goes wrong, if medication is missed or doubled, if behaviour changes and there’s no note—where’s the evidence? Where’s the accountability?
Where Is the Care?
This situation isn’t about one support worker, or even one provider. It speaks to a wider issue in some corners of the disability support sector:
- Where is the care to train staff properly?
- Where is the care to build systems that protect the participant, not just the provider?
- Where is the care to document, not because it’s a requirement—but because it’s the right thing to do?
When the basics are ignored, it’s the participant who suffers. Their well-being. Their trust. Their safety.
We can’t keep pretending this is acceptable. Because it’s not.
Medication Administration: There Are Rules for a Reason
There are seven essential rights when it comes to safe medication administration. Every disability support worker should know them,and every provider should enforce them:
- Right person
- Right medication
- Right dose
- Right time
- Right route
- Right reason
- Right documentation
When even one of these goes unchecked, the whole system is at risk.
Documentation isn’t just paperwork. It’s protection,for the participant, for the support worker, and for the provider. It builds a chain of accountability. It shows patterns. It tells the story of care. And most importantly, it prevents harm.
What Needs to Change?
Providers must stop seeing documentation as an afterthought. It’s a critical part of safeguarding participants, particularly those with complex support needs.
Here’s what every registered NDIS provider should be doing:
- Mandatory medication training for all staff who administer or witness medication use.
- Clear medication administration records (MARs) kept daily—signed, dated, and stored properly.
- Regular audits and spot checks to ensure documentation and processes align with best practice.
- Shift notes completed consistently, with meaningful updates on the participant’s health, behaviour, and support.
We Can—and Must—Do Better
This isn’t just about compliance. It’s about dignity, safety, and respect.
NDIS participants deserve more than “good enough.” They deserve a system built on clarity, communication, and care, especially when it comes to medication.
If you’re a provider, a coordinator, or a family member, now is the time to ask the hard questions:
- Is medication being tracked properly?
- Are staff fully trained and supported?
- Do our systems serve the person,or just tick the boxes?
If the answer isn’t clear, it’s time to change that.
If you’re unsure whether your current supports meet medication safety standards, or if you’d like guidance on what best practice should look like, contact SEQ Disability Support for confidential advice or to make an enquiry—because safe, accountable care should never be optional.